Epidemiologic studies indicate that ever larger numbers of people report having sensitive skin, for which a European prevalence of 50% is estimated. Sensitive skin is characterized by hyperreactivity, with manifestations varying in relation to many factors. The pathogenesis of this disorder is poorly understood, although studies point to a biophysical mechanism. Objective diagnosis of sensitive skin is difficult, as information comes mainly from the patient's report of symptoms in the absence of effective, strongly predictive tests because of great interindividual variability in skin sensitivity. Substances that trigger a reaction in hypersensitive skin also vary greatly. The impact of this syndrome on quality of life is considerable and patients often present psychiatric symptoms; therefore, dermatologists should explore this possibility when taking a patient's history. Patient cooperation and physician persistence are both essential for treating sensitive skin.
Los estudios epidemiológicos ponen de manifiesto que cada vez son más las personas que dicen poseer una piel sensible, presumiéndose una prevalencia del 50% en la población europea. Se trata de una condición cutánea de hiperreactividad cuya manifestación depende de gran variedad de factores y cuya patogénesis no es del todo conocida, aunque diferentes estudios señalan un origen biofísico para este desorden. El diagnóstico objetivo de piel sensible es difícil, ya que la mayoría de los síntomas que presentan los pacientes son subjetivos. Además, no existen pruebas diagnósticas realmente eficaces y con un fuerte componente predictivo, pues la sensibilidad de la piel varía mucho de unas personas a otras. Por otra parte existen numerosas variaciones entre los compuestos que desencadenan respuestas del tipo de piel sensible. Las repercusiones sobre la calidad de vida son importantes y frecuentemente se acompañan de sintomatología psiquiátrica, por lo que el médico dermatólogo debe explorar este campo en la anamnesis. En el tratamiento de esta condición se hace imprescindible la colaboración del paciente y altas dosis de tenacidad por parte del médico.
While the term sensitive skin has several synonyms in the scientific literature, including intolerant skin, reactive skin, and hyperreactive skin, for the purpose of this review, we will use the most widely used term: sensitive skin.1
DefinitionAlthough the term sensitive skin first appeared decades ago, it was used only sporadically and was barely mentioned in the scientific literature until a few years ago.2 Since then, however, it has been appearing with increasing frequency. Sensitive skin, however, is still a condition that is difficult to define and diagnose. While numerous definitions have been proposed over the years, none have provided an accurate, unambiguous description of this condition.3
For some authors, sensitive skin refers to “an exaggerated and unpleasant sensitivity of the skin to frequent or prolonged use of everyday products such as cosmetics or toiletries”.4 For others, it is the individual perception of the patient that their skin reacts in an exaggerated manner to different stimuli including environmental factors and topically applied products.5 For Ständer et al,6 it is a skin condition rather than a disease entity, while for Chew and Maibach7 it is “not a single entity but a heterogeneous syndrome puzzling both consumer and clinician alike”. Kligman et al8 resolutely stated that sensitive skin was “a biological reality as valid as other cutaneous disorders, which seem to consist mainly of subjective complaints”. Finally, Pons-Guiraud9 considered sensitive skin to be a complex phenomenon that both patients and physicians found difficult to identify, quantify, and manage.
Health-related quality of life (HRQOL), that is, a patient's perception of their physical, mental, and social health, is very often impaired in patients with sensitive skin.1,6,10,11
In conclusion, sensitive skin can be defined as a complex condition that (1) is characterized by high subjective sensitivity, (2) can present with or without clinical symptoms, (3) can appear alone or in association with other skin conditions, and (4) has a considerable impact on HRQOL.
Epidemiological DataPrevalenceThe scientific literature shows a worldwide increase in the prevalence of sensitive skin in recent years.4,9,12–15
The estimated prevalence in Japan, Europe, and the United States is 50% among women and 30% among men, with a similar distribution across countries and continents.6
In a telephone survey conducted in several European countries (France, Italy, Portugal, Germany, Switzerland, Belgium, and Greece), 37.6% of those interviewed (n=4506) reported having sensitive or very sensitive skin.13
Sensitive skin is also very common in Spain, with over 11 million Spaniards (35.4% of women and 27.9% of men) claiming that they have sensitive or very sensitive skin.16
SexMany studies have investigated possible associations between sensitive skin and sex, race, or age,4,6 but with inconsistent results.6
With respect to sex-related differences, the general perception is that more women claim to have sensitive skin than men,2,4 but some authors have reported a significantly higher prevalence among men.6
Farage2 reported that the perceived severity of sensitive skin was comparable in men and women, but that men perceived less severe reactions on the face. She also found that men and women cited different causes for their condition, with 15% of women and 11% of men linking it to irritation due to cosmetic products, and 9% of men and just 4% of women linking it to contact as a result of friction or rubbing.
Shaving appears to be the most common factor associated with sensitive skin in men. In a study conducted in France, 41% of men interviewed reported sensitive skin symptoms after shaving.17
An interesting association has been detected between sensitive skin and urinary incontinence in women, with one epidemiological study showing a significantly higher proportion of women over 50 years old with light urinary continence claiming to have sensitive skin compared to a control group matched for age and sex.18 Interestingly, the women with incontinence (n=29) but not the controls reported less skin sensitivity in the genital area than overall.
RaceSeveral studies have suggested that black people have less sensitive skin than white people, and that white people, in turn, have less sensitive skin than Asians. There is, however, no statistical evidence to support these hypotheses, and the differences that have been detected between different ethnic groups are probably not race-related but rather due to pyschosocial4 and cultural factors4,6 (eg, personal hygiene practices4,6 and diet). Asians, for example, have stronger skin reactions to spicy food.6 Two studies have evaluated the intensity of reactions to capsaicin in different ethnic populations. In the first study, African Americans showed a limited hypersensitivity after the topical application of capsaicin (no significant changes in heat detection threshold, pain intensity, or skin blood flow), while East Asian, Hispanic, and white participants experienced significant changes in hyperalgesia and vasodilatation.19 In the second study, only minimal differences were detected between Asian, African, and white women in the capsaicin skin neurosensitivity test.20
AgeAge can have a considerable influence on susceptibility to sensitive skin, and some studies suggest that young people are more prone than older people. In a study carried out in France, 52% of 1006 individuals reported having sensitive skin.6
The data support the observation that sensitive skin is a common condition and that its frequency decreases with age.17
The lack of studies analyzing sensitive skin in children is noteworthy, particularly considering the growing number of personal care products on the market specifically targeting this population.4 Indeed, the medical literature contains no analyses of sensitive skin in children.4 It should also be noted that the body surface area to body mass ratio is very high in children, which means that they are subject to high exposure to skincare products21 and therefore possibly more prone to sensitive skin.
EtiologyThe etiology of sensitive skin is multifactorial, involving an underlying genetic susceptibility combined with exogenous and endogenous factors that can trigger or aggravate the clinical expression of the condition.9
Endogenous FactorsInherent FactorsSensitive skin is associated with the following inherent qualities4:
- 1.
Female sex
- 2.
Youth
- 3.
Susceptibility to blushing and/or flushing
- 4.
Skin pigmentation
- 5.
Thin stratum corneum
- 6.
Decreased hydration of stratum corneum
- 7.
Disruption of stratum corneum
- 8.
Increased epidermal innervation
- 9.
Increased sweat glands
- 10.
Increased neutral lipids and decreased sphingolipids
- 11.
High transepidermal water loss (TEWL)
An association has also been observed between skin type and sensitivity. From the cosmetic standpoint, there are 4 types of healthy skin: normal, oily, dry, and mixed. Several authors, however, have proposed a fifth category: sensitive skin.
In an opinion poll conducted in Europe, 14.2% of respondents with sensitive skin said that they had dry skin, 11.1% said that they had oily skin, and 4% said that they had normal skin.13 That study detected a statistically significant association between cosmetic skin type and sensitive skin.
Skin phototype also appears to be associated with sensitive skin and has been reported to have a significant impact on perceived sensitivity, with phototype I being most commonly associated with sensitive skin.10
Associated FactorsClassic studies have detected associations between sensitive skin and seborrheic diathesis, atypical psoriasis, rosacea, perioral dermatitis, erythro-couperosis, and atopic dermatitis.9
In a European study of sensitive skin conducted by Misery et al,13 12.6% of the population studied reported a concomitant skin condition. The most common conditions mentioned were acne, contact dermatitis, psoriasis, rosacea, atopic dermatitis, seborrheic dermatitis, and vitiligo.
The above data suggest that sensitive skin is often associated with other skin diseases, but that it is difficult to determine whether the symptoms of a patient with sensitive skin are due to the concomitant skin disorder or whether there is an association between the skin disorder and sensitive skin.13
Sensitive skin has also been linked with atopy,4,13 and indeed atopic dermatitis has been cited as the condition that most commonly predisposes to sensitive skin. A study conducted in 25 Greek women with atopic dermatitis found a significant association between clinically diagnosed atopic dermatitis and perceived skin sensitivity, with all the patients in the group stating that they had sensitive skin, albeit to varying degrees.23 Indeed, 80% claimed to have moderately sensitive or very sensitive skin. The same study revealed the hereditary component of sensitive skin as, compared to the control group, a significantly higher proportion of patients with atopic dermatitis reported having a relative with sensitive skin.
An association has also been demonstrated between atopic dermatitis and stinging (a sensation between discomfort and pain, similar to that described for a burn), with a higher skin nerve density detected in individuals with atopic skin than with normal skin.24
Patients with respiratory atopy and active rhinoconjunctivitis have also been observed to have increased skin sensitivity to diverse irritants.25
In view of the above, several authors consider that atopic dermatitis is a multifactorial disease that affects patients with epidermal barrier dysfunction and dry, sensitive skin.26
Finally, certain cases of sensitive skin appear to be a subclinical expression of allergic contract dermatitis, although these are extremely rare.8
Exogenous FactorsThe use of cosmetics that are unsuitable for a particular skin type is the most common exogenous factor that can trigger sensitive skin.9
Cosmetics and ToiletriesMany cosmetic formulations contain alcohol, propylene glycol, butylene glycol, cocamidopropylbetaine, triethanolamine, resorcine,22 trichloroacetic acid, and alpha hydroxy acids, which, depending on their concentration, have a greater or lesser irritant effect and can aggravate sensitive skin.9 Topical corticosteroids increase skin fragility and cause chronic, localized erythema, leading to increased cosmetic intolerance and possibly triggering symptoms of sensitive skin in the affected area.4,9 UV-A exposure and surgical or nonsurgical cosmetic procedures, such as phototherapy, dermabrasion, laser resurfacing and facelifts, can all aggravate sensitive skin.9
Environmental FactorsA number of environmental factors that trigger sensitive skin reactions have been identified,10,14 including heat and cold, sun, wind, pollution, and air-conditioning.4,6 It is known that the decrease in temperature and humidity levels that typically occur in winter and in cold environments reduce the water content of the stratum corneum3 and favor the expression of sensitive skin symptoms.
Other, lifestyle-related environmental factors, are
PathophysiologySkin sensitivity is a complex process in which a range of pathophysiological phenomena have been observed.
Roussaki-Schulze et al,27 for example, in a study comparing sensitive skin and nonsensitive skin, described the following objective biophysical findings in the group of individuals with sensitive skin:
- 1.
Very dry skin with low fatness, which leads to a disturbance of the protective skin barrier function
- 2.
Hyperreaction of the skin blood vessels
- 3.
Increased transcutaneous penetration of water-soluble chemicals
- 4.
Enhanced immune responsiveness
- 5.
Significant decrease of alkali resistance
- 6.
Heightened neurosensory stimulation
Based on the results of these and other studies the pathophysiology of sensitive skin has been classified into a number of categories, discussed below.
Low Skin Tolerance ThresholdA reduction in the skin's tolerance threshold not directly related to immunologic or allergic mechanisms has been observed in individuals with sensitive skin.5
Furthermore, the wide variety of sensory symptoms that have been identified in these individuals suggests sensory dysfunction of the nerves of the skin5 and a lowering of the nerve response threshold.6 Inadequate protection of nerve endings4 leads to increased sensitivity to irritants and exogenous stimuli.9
The mechanism that triggers the nerve response is reflected in modified cerebral activity. A study in which women underwent a simple blind test involving the application of lactic acid to the nasolabial fold while being monitored by magnetic resonance imaging, revealed the existence of a specific response in the central nervous system, suggesting that the excitability mechanism in sensory epidermal nerves on the face triggers cerebral activity that is very similar to that observed in skin pain processes.5
Recent studies have shown that the transient receptor potential vanilloid 1 (TRPV1) contributes to the expression of sensitive skin symptoms by facilitating neurogenic inflammation and leading to hyperalgesia.30
Muizzuddin et al28 found that skin of East Asians, and of whites to a certain extent, was characterized by low maturation and a relatively thin skin barrier, while that of African Americans was characterized by low ceramide levels and high cohesion in the upper layers of the stratum corneum.28 Those authors suggested that these differences might explain the disparity between East Asians and African Americans in the prevalence of sensitive skin.
Another study in patients with sensitive skin detected a correlation (r[s]=-0.47; P<.001) between the intensity of symptoms and the irregularity skin index.29
Altered Skin Barrier Function5It has been established that the abnormal penetration of irritant substances into the skin due to altered barrier function triggers the symptoms of sensitive skin.9
Results obtained using a recently developed procedure based on the plastic occlusion stress test and measurement of TEWL desorption curves to assess skin barrier integrity in individuals with sensitive skin support the hypothesis that skin sensitivity is associated with greater barrier function impairment.31
Increased Permeability (TEWL)5Impaired skin barrier function increases the permeability of the stratum corneum.4,6,9
Altered Intercellular LipidsAlterations in intercellular lipids have also been reported in disorders such as atopic dermatitis and seborrheic dermatitis, in which the skin tolerance threshold is reduced by alterations in intercorneocytic lipids9; the stratum corneum is also thinner in such cases.4,9
Clinical ManifestationsBased on the definition provided at the beginning of this review, sensitive skin is associated with the characteristics described below.
High Subjective SensitivityIndividuals with high subjective skin sensitivity experience an almost continuous sensation of tingling, burning, stinging, and tightness of the skin,32 although the intensity of symptoms varies greatly from one individual to the next.
Variations in sensitivity by anatomic site have also been identified.33 While the face is the most common site for sensitive skin,6 a study by Saint-Martory et al34 found that other parts of the body are also affected, namely the hands (58%), the scalp (36%), the feet (34%), the neck (27%), the torso (23%), and the back (21%). The above findings are supported by the results of studies that have identified neurosensory and physiological differences in the skin of different parts of the body.4
- 1.
The face. In a study by Farage33 in 2009, 77.3% of individuals with sensitive skin claimed that they had sensitive facial skin; the percentages for those reporting sensitive body skin and sensitive genital skin were 60.7% and 56.3%, respectively. The only significant difference found on analyzing the results by sex, ethnic origin, and age was that a higher proportion of women and African Americans reported sensitive skin in the genital area. The facial area is probably affected most by sensitive skin because of the high number of cosmetic products used on the face and the fact that it has a weaker skin barrier than other parts of the body as well as a large number of nerve endings.12 The nasolabial fold is considered to be the most sensitive part of the face due to the permeability of its stratum corneum, its high density of sweat glands and hair follicles, and its rich innervations.4 The next most sensitive areas are the malar eminence, the chin, the forehead, and the upper lip.13
- 2.
The scalp. Misery et al35 assessed scalp sensitivity in a sample of 1011 individuals; of these, 44.2% claimed that they had a sensitive scalp, and within this group, 11.5% had a scalp disease. There was a significant association between hair loss and scalp sensitivity. Prickling, itching, and pain were more common in the sensitive skin group, and the main triggers were pollution, heat, emotions, and shampoo. The authors found no association between scalp sensitivity and skin sensitivity in other parts of the body. Based on their findings, Misery et al. concluded that scalp sensitivity was a genuine, common condition. A subsequent study reported that the most common symptoms associated with sensitive scalp were itching and tingling and also stated that dandruff could not be considered a symptom of sensitive skin.36
- 3.
The vulvar region. The vulvar region has particular anatomic characteristics that appear to make it more prone to irritation, but as Farage and Maibach12 have indicated, there is very little evidence supporting an association between female hygiene products and sensitive skin. In another study, Farage37 remarked that while topical agents frequently cause vulvar irritation, their irritant action is often underestimated. In a group of patients with chronic vulvar irritation, 29% were found to have contact hypersensitivity, while 94% reported secondary sensitization to topical medication.38 As concluded by Farage and Maibach,12 vulvar sensitivity is often related to contact hypersensitivity, which, in turn, is related to the use of topical medication and hygiene products.
Sensitive skin is associated with a wide range of nonspecific clinical signs, including erythema, telangiectasis, and scaling.3,32,39
Presence or Absence of Associated ConditionsIndividuals with sensitive skin can also present clinical signs typically associated with concomitant conditions such as acne, contact dermatitis, psoriasis, rosacea, atopic dermatitis, seborrheic dermatitis, and vitiligo.
Impact on Quality of LifeSensitive skin has considerable psychological effects, and has been seen to adversely affect quality of life, with greater impairment seen in individuals with more sensitive skin.10 Zafiriou et al11 observed an association between skin hypersensitivity and somatization, anxiety, phobic anxiety, hostility, and interpersonal sensitivity.
Clinical VariantsThree clinical variants of sensitive skin, each with different symptom intensity, have been identified:
- 1.
Very sensitive skin (dry or fatty)9 or intrinsic skin;5 both types react strongly to exogenous factors (eg, environmental insults) and endogenous factors. The symptoms are acute and permanent and tend to have psychological effects.9
- 2.
Environmentally sensitive skin. This is often clear, dry, thin skin that essentially reacts to environmental factors such as heat and abrupt temperature changes.9
- 3.
Cosmetically sensitive skin. This is mildly sensitive skin that mainly reacts to cosmetics that are generally easy to identify.9
Sensitive skin was seldom diagnosed in the past, possibly because, as Farage and Maibach suggested, many dermatologists considered it to be a princess and pea phenomenon.12 Its high prevalence, however, has made it necessary to establish valid diagnostic criteria.
Misery et al13 recommend that dermatologists regularly ask their patients whether they have sensitive skin.
The syndrome is generally self-diagnosed and is characterized by a wide range of symptoms of greatly varying intensity. Furthermore, the fact that numerous factors are involved in its origin makes it difficult to establish a clinical diagnosis.4
Kligman et al8 described different definitions of sensitive skin which, in their opinion, facilitate diagnosis. These are as follows:
- 1.
Subjective irritation: irritant response without visible clinical signs
- 2.
Neurosensory irritation: neurally mediated responses such as itching, stinging, burning, tightness
- 3.
Chemosensory irritation: sensory responses induced by chemicals in contrast to physical, mechanical and environmental factors
- 4.
Psychophysical irritation: irritation with a psychological component.
However, to facilitate diagnosis, patients must complete questionnaires and undergo physical tests that will provide information on these aspects of sensitive skin.
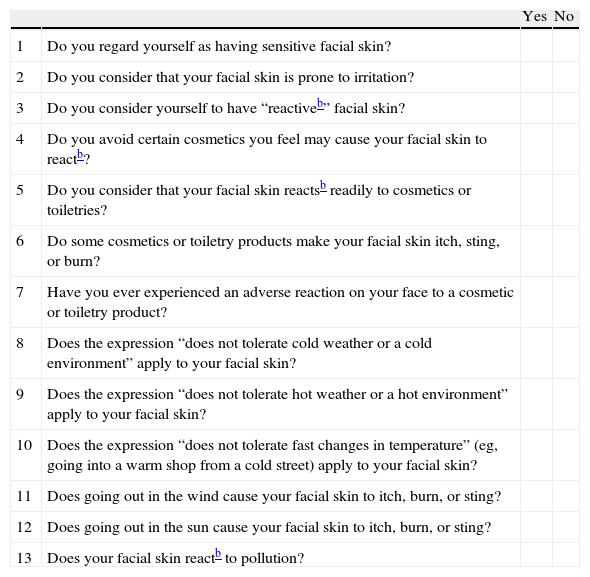
QuestionnairesOne of the questionnaires used to evaluate sensitive skin was designed by Querleux et al. (Table 1)5; the questions are related to the typical characteristics of very sensitive skin and contemplate reactions due to the topical application of personal hygiene products and environmental factors.
Questionnaire to Identify Individuals With Sensitive Skina.
| Yes | No | ||
| 1 | Do you regard yourself as having sensitive facial skin? | ||
| 2 | Do you consider that your facial skin is prone to irritation? | ||
| 3 | Do you consider yourself to have “reactiveb” facial skin? | ||
| 4 | Do you avoid certain cosmetics you feel may cause your facial skin to reactb? | ||
| 5 | Do you consider that your facial skin reactsb readily to cosmetics or toiletries? | ||
| 6 | Do some cosmetics or toiletry products make your facial skin itch, sting, or burn? | ||
| 7 | Have you ever experienced an adverse reaction on your face to a cosmetic or toiletry product? | ||
| 8 | Does the expression “does not tolerate cold weather or a cold environment” apply to your facial skin? | ||
| 9 | Does the expression “does not tolerate hot weather or a hot environment” apply to your facial skin? | ||
| 10 | Does the expression “does not tolerate fast changes in temperature” (eg, going into a warm shop from a cold street) apply to your facial skin? | ||
| 11 | Does going out in the wind cause your facial skin to itch, burn, or sting? | ||
| 12 | Does going out in the sun cause your facial skin to itch, burn, or sting? | ||
| 13 | Does your facial skin reactb to pollution? |
Misery et al35 proposed the 3S questionnaire as an appropriate, effective tool for assessing the severity and symptoms of scalp sensitivity.
Physical TestsMany attempts have been made to find a test capable of providing an objective diagnosis of sensitive skin, but none of the tests analyzed have proven to be sufficiently effective, highlighting, once again, the subjective nature of sensitive skin.3,9
Farage et al4 reviewed the available tests for the assessment of sensitive skin and classified them into 3 major groups: (1) those that assessed neurosensory responses (sensory reactivity tests); (2) those that assessed visible signs of skin irritation (irritant reactivity tests); and (3) those that measured structural and physiological parameters of the skin as indicators of the irritant effect (dermal function tests).4
The stinging test designed by Frosch and Kligman40 is considered to be the most effective. It involves the application of 0.5mL of 10% lactic acid to one nasolabial fold and distilled water at room temperature to the other. The symptoms, assessed subjectively, are scored on a scale of 1 to 4 according to intensity.6,9 Other substances used in this test are capsaicin, ethanol, menthol, sorbic acid, and benzoic acid.4,9 The stinging test is considered to be the best way to diagnose sensitive skin.4,9 Furthermore, it is fast, cheap, and simple,4 although most authors generally agree that it lacks predictive value. Marriot et al39 indicated that a positive stinging test result in the nasolabial fold does not necessarily predict subjective responses to products applied to other parts of the face.
The plastic occlusion stress test combined with the measurement of TEWL desorption curves provides a more objective assessment of sensitive skin.31 It is a new, dynamic approach, which, unlike baseline TEWL measurements, provides unequivocal evidence of skin barrier impairment.31 Accordingly, it would seem that this test could be used to diagnose or predict sensitive skin.31Pons-Guiraud9 recommends including cosmetics and personal care products used by patients in allergy tests to detect subclinical manifestations of contact allergy. Should any signs of sensitive skin be detected, the author recommends withdrawing all cosmetics and reintroducing them, one by one, at 2-week intervals, and notes that it is important to limit the type of cosmetics used and the frequency with which these are applied in the final stage of the program.9
Treatment and PreventionSensitive skin is difficult to manage for both dermatologists and patients because the reactions are subjective, vary from one individual to the next, and can be triggered by many different factors.
Sensitive skin is also a challenge for the cosmetics industry, where the key to ensuring patient well-being lies in the identification of appropriate dermatologic treatments and a rational approach to the selection of cosmetic products.41
Medical TreatmentTopical corticosteroids are the most effective medical treatment for sensitive skin, although they must be used in moderation due to the risk of adverse effects such as skin thinning and impairment of skin barrier function.42
Topical calcineurin inhibitors are also effective. While they do not cause the adverse effects observed with corticosteroids, they are associated with numerous adverse reactions, such as itching and burning at the application site, although these tend to be mild and transient.42
Cosmetic TreatmentThere are numerous cosmetic treatments available for sensitive skin. Muizzuddin et al43 found that the use of products containing minimal preservatives and no surfactants for 8 weeks led to a change in the characteristics of sensitive skin, with improved skin barrier function and similar reactivity to that seen in nonsensitive skin. Moisturizers have also been seen to have a positive effect on sensitive skin as they improve skin hydration, reduce susceptibility to irritation, and restore the integrity of the stratum corneum.44
Draelos41 and Pons-Guiraud9 recommend the use of products specially designed for sensitive skins; these contain few ingredients and irritants and no common sensitizers or cutaneous sensory or vasodilatory stimulants.
Advances have been made in recent years on a new treatment approach involving a novel bioactive, trans-4-tert-butylcyclohexanol. Kueper et al30 described how this selective transient receptor potential cation channel subfamily V member 1 (TRPV1) antagonist was capable of inhibiting capsaicin-induced activation. The authors found that 0.4% trans-4-tert-butylcyclohexanol significantly reduced capsaicin-induced burning in a clinical study of 30 women tested with a topical emulsion containing 31.6ppm of capsaicin.
HydrationTreatment with Rhodiola rosea extract/l-carnosine–associated compound (RCAC) has been seen to protect skin barrier function and improve subjective responses in patients with sensitive skin.45
The effectiveness of this compound was demonstrated in a study by Dieamant et al45 by a reduction in TEWL, an improvement in hydration and the sensation of skin comfort, and a reduction in stinging test discomfort. The authors showed, in vitro, that the positive in vivo responses were due to a significant increase in the release of opioid peptides, an inhibitory effect on the production of neuropeptides, and the modulation of cytokine production by keratinocytes subject to ultraviolet stress.
Cleansing AgentsSoap is one of the toiletry products that cause most skin reactions, and the problem is particularly acute among individuals obliged to wash their hands frequently. In such case, dermatologists need to recommend suitable cleansers,46 and the best choice appears to be an alcohol gel with moisturizer. These gels are designed to maintain skin barrier integrity, relieve dryness, and restore barrier function. The combined use of soap-free cleansers and topical treatments has been shown to lead to clinical improvement in patients with sensitive skin.44
Antiaging CreamMerinville et al47 proposed using sodium salicylate instead of salicylic acid in antiaging creams for sensitive skins; salicylic acid, which is usually present in high concentrations in antiaging products, can cause adverse effects such as somatosensory and visible irritation. Those authors reported that, compared to placebo, sodium salicylate caused a significant increase in fibrillin and collagen-1 antiaging biomarkers and significantly reduced wrinkle depth and skin redness after 4 and 8 weeks of daily application.
It has been suggested that hydroxy acids, which are a common ingredient in antiaging creams and are considered to be strongly irritant for sensitive skin, should be replaced by polyhydroxy and bionic acids as these offer the same benefits as hydroxy acids but do not cause skin irritation; furthermore, they provide additional antioxidants, strengthen the skin barrier, and have moisturizing effects.48
Preventive TreatmentNeukam et al49 recommended dietary supplementation with flaxseed oil as preventive treatment for sensitive skin. They showed that this supplement significantly reduced sensitivity after nicotinate irritation, skin redness and scaling, and also improved smoothness and hydration.
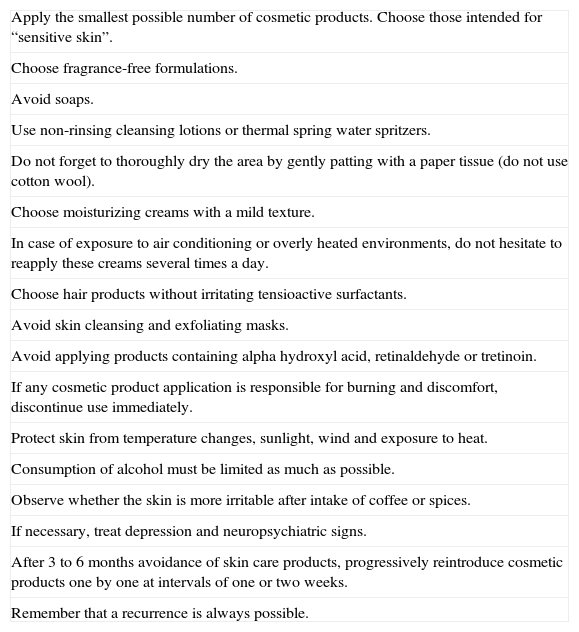
Pons-Guiraud9 has recommended a set of guidelines for the prevention and management of sensitive skin (Table 2).
Treatment Guidelines Recommended by Pons-Guirauda.
| Apply the smallest possible number of cosmetic products. Choose those intended for “sensitive skin”. |
| Choose fragrance-free formulations. |
| Avoid soaps. |
| Use non-rinsing cleansing lotions or thermal spring water spritzers. |
| Do not forget to thoroughly dry the area by gently patting with a paper tissue (do not use cotton wool). |
| Choose moisturizing creams with a mild texture. |
| In case of exposure to air conditioning or overly heated environments, do not hesitate to reapply these creams several times a day. |
| Choose hair products without irritating tensioactive surfactants. |
| Avoid skin cleansing and exfoliating masks. |
| Avoid applying products containing alpha hydroxyl acid, retinaldehyde or tretinoin. |
| If any cosmetic product application is responsible for burning and discomfort, discontinue use immediately. |
| Protect skin from temperature changes, sunlight, wind and exposure to heat. |
| Consumption of alcohol must be limited as much as possible. |
| Observe whether the skin is more irritable after intake of coffee or spices. |
| If necessary, treat depression and neuropsychiatric signs. |
| After 3 to 6 months avoidance of skin care products, progressively reintroduce cosmetic products one by one at intervals of one or two weeks. |
| Remember that a recurrence is always possible. |
Importantly, all treatment approaches should include the recommendation to avoid, where possible, triggers of sensitive skin symptoms, and, as Pons-Guiraud has stated, this requires “cooperation from the patient and tenacity from the physician”.9
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors would like to thank Rocío Segura Rodríguez for her assistance with bibliographic documentation.
Please cite this article as. Escalas-Taberner J, et al. La piel sensible : un síndrome complejo. Actas Dermosifiliogr.2011;102:563-571.